According to the Agency for Healthcare Research and Quality, up to one million patients fall in the hospital each year — and according to Tom Hoover, registered nurse and IT clinical analyst at Memorial Health Care Systems (MHCS) (Seward, Nebraska), “If you have one fall, that’s too many.”
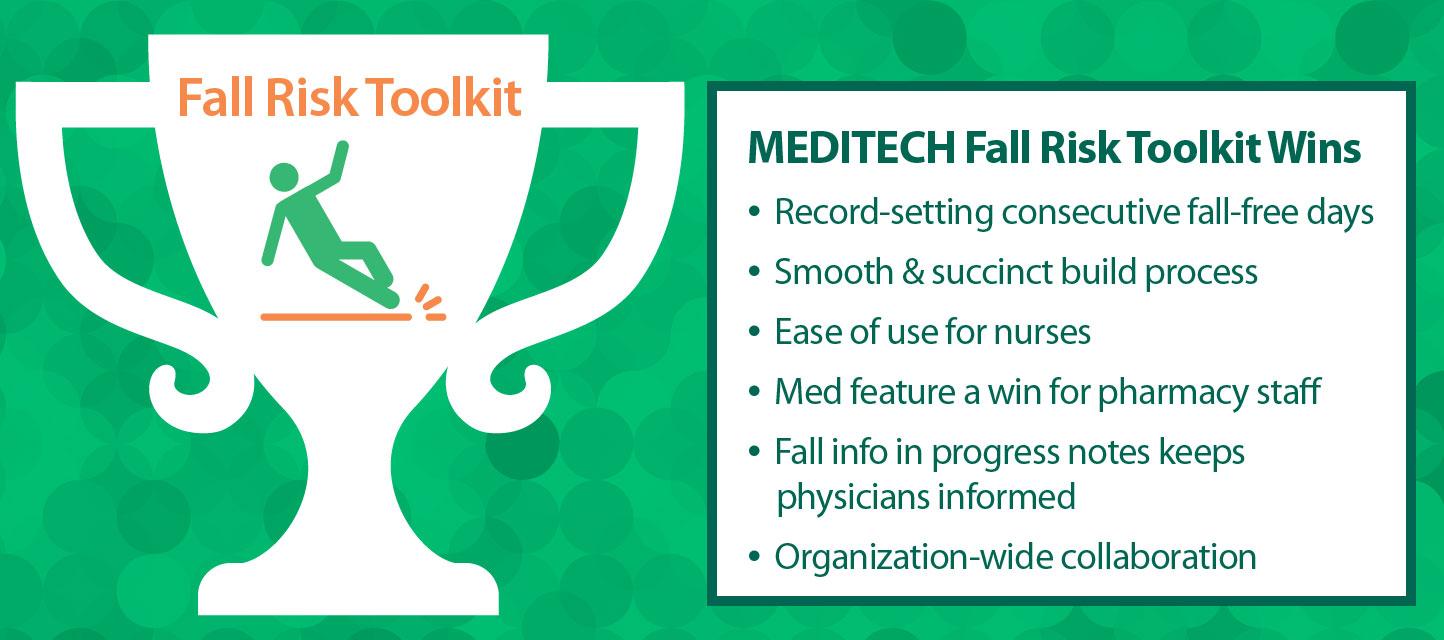
MHCS went LIVE with MEDITECH’s Fall Risk Management Toolkit on March 26, and April 26 marked 30 concurrent days without injury in their facility.
To implement the toolkit, Hoover said everyone must be on board — “it truly is an organizational effort.” MHCS created a multidisciplinary Falls Team that included housekeeping, physical therapy, and pharmacy alongside nursing staff, to review the toolkit and determine which workflow changes would produce desired outcomes. The entire process from planning to LIVE — including TEST and LIVE build, an iterative testing process to ensure optimal workflow, and staff education — took just under three months. Detailed documentation, such as step-by-step screen shots to highlight differences between areas (ED, critical access, etc.), introduced nursing staff to new workflows.
Other marketing efforts included a formal kickoff and the addition of posters and signage throughout patient rooms. Hoover noted the purpose of this being twofold — to shift the culture to increase fall risk awareness and to emphasize hospital-wide responsibility of the issue. “This is everyone’s responsibility,” he said. “If you’re walking down the hall and you see that yellow light on above the door indicating a fall risk and the patient is walking around, go in there to stand with them and yell for help.”
Once they went LIVE with the toolkit, MHCS made further modifications to fit the needs of their care providers’ daily workflows. For example, based on nurse feedback and stakeholder buy-in, the education piece of the toolkit assessment was removed completely and instead made its own document. “The expectation for falls education is a sit-down formal discussion about patient safety and falls — it’s not meant to be done every shift. The language and the build part is identical to what’s in the toolkit, but it’s now separated out and set to once PRN.” As an early adopter, Hoover was able to relay this recommendation back to MEDITECH for consideration, which has been incorporated into the toolkit FAQs.
Overall, MHCS staff appreciate efficiencies brought forth by the toolkit, including the fact that the new workflow meets standards for fall prevention. Nursing staff also enjoy the ease of use — especially the embedded algorithm that evaluates a patient's medication list to determine if a Pharmacy consult is warranted. Hoover anticipates a positive impact on patient safety by bringing Pharmacy into the loop for early evaluation. Likewise, physicians benefit by having fall risk details automatically populate their progress notes so they’re aware of the patient’s risk of falling and precautions being taken.
In terms of staff being resistant to the new process, Hoover said, “Workflows can change — change is not bad. We’re all here to provide quality care. Regardless of the processes that are in place or have been in place, complacency is dangerous. By using the technology available to us to help us make decisions and track outcomes, including our quality and the services we provide, it’s something that you need to continue to strive for.”
Hoover said working with MEDITECH has been an “awesome experience.” Implementing the Fall Risk EHR Toolkit enabled MHCS to “integrate departments that hadn’t worked together before, and it’s opened up opportunities for other collaborative projects.”